Share and Follow
Experiencing dry, gritty eyes after age 50 can make everyday activities like reading or driving quite uncomfortable. While many attribute these symptoms to the natural aging process, medical professionals are increasingly identifying ocular rosacea as a significant, yet often overlooked, cause affecting millions of individuals.

What Is Ocular Rosacea?
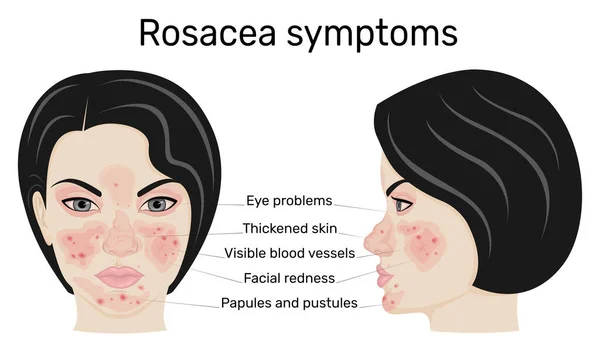
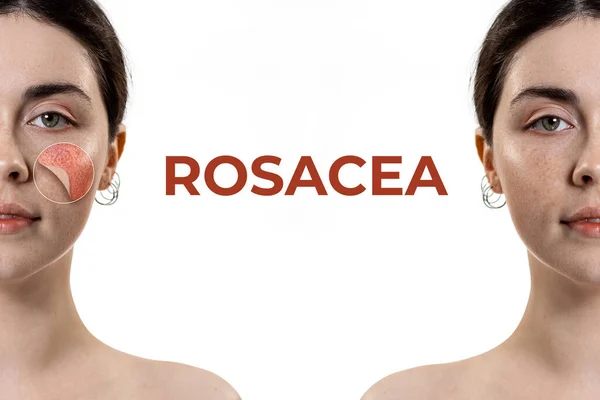
Ocular rosacea is characterized by chronic inflammation of the eyes and eyelids, frequently linked to its skin counterpart. “Ocular rosacea often occurs alongside cutaneous rosacea,” explains board-certified NYC cosmetic dermatologist Dr. Michele S. Green. This condition presents as redness, burning, and the sensation of a foreign body in the eye, primarily due to meibomian gland dysfunction and blepharitis. Symptoms include visible small blood vessels on the eyelid margins and gland blockages, leading to evaporative dry eye. Without treatment, it can lead to chalazia, corneal ulcers, or scarring. Unlike typical dry eye, ocular rosacea arises from vascular dysregulation and an overactive immune system, making eyes more sensitive to triggers like heat or stress. For instance, Sarah, a 55-year-old teacher, initially mistook her persistent eye irritation for allergies until she was diagnosed with gland blockages. Statistics indicate that this condition affects over 16 million Americans with rosacea, with ocular symptoms present in up to 58% of cases. Early detection is crucial to prevent vision impairment, as severe inflammation can blur vision.
Why Does It Strike After 50?
Hormonal changes during midlife can worsen vulnerabilities in vascular and immune systems. After menopause, declining estrogen levels destabilize the tear film, exacerbating pre-existing gland dysfunction caused by genetic or environmental factors. This age group often encounters a range of triggers, such as sun exposure, caffeine, or spicy foods, which can lead to flushing and inflammation. Research has also connected ocular rosacea to Helicobacter pylori or eyelash mites (Demodex), which thrive as skin barriers age. One survey revealed that 70% of rosacea patients over 50 experience ocular symptoms, compared to 40% of younger patients. The condition’s neurovascular dysregulation becomes more pronounced as nerve hypersensitivity increases the sensation of burning. It’s akin to a dam finally breaking after years of gradual blockage, resulting in gritty discomfort. Experts also highlight that environmental extremes and certain medications, like beta-blockers, heighten the risk after age 50.
4 Expert-Backed Ways to Ease Symptoms
Warm Compress
To alleviate symptoms, applying a warm compress daily can help unclog meibomian glands and restore oil flow to the tears. Simply soak a clean cloth in warm (not hot) water for about 10 minutes, twice a day. This straightforward practice reduced symptoms by 60% in one study, offering a drug-free way to manage inflammation.
Oral Antibiotics
For more moderate cases, treatments such as doxycycline or azithromycin can target bacterial overgrowth and cytokines, helping to reduce flare-ups. Low-dose regimens (20-40mg daily) are designed to minimize side effects while managing immune system overactivity. Many patients report an 80% improvement in redness and dryness after three months of treatment.
Meibomian Gland Probing
This in-office procedure uses fine probes to clear hardened secretions, often under local anesthesia. Performed by ophthalmologists, it yields lasting relief; trials show 75% of patients regain gland function. Pair with lid hygiene for best results.
Intense Pulsed Light Therapy (IPL)
IPL targets telangiectasia and inflammation via light pulses on eyelids. Sessions (4-6 over months) close abnormal vessels, boosting tear quality—studies report 87% symptom reduction. It’s non-invasive, with minimal downtime.
Can Ocular Rosacea Be Cured?
No cure exists, as it’s chronic, but management halts progression. This lifelong condition demands ongoing care to prevent corneal damage. Lifestyle tweaks—avoiding triggers like alcohol or dairy—sustain remission.
What New Research Shows
Recent 2025 studies highlight TLR-targeted therapies and microbiome modulators. One trial with novel anti-inflammatory peptides cut flare frequency by 65%. Probiotic eyedrops show promise in restoring ocular flora, per PubMed reviews. Future directions include personalized IPL with AI gland mapping, offering hope for sustained control. These advances underscore early intervention’s role in preserving vision.