Share and Follow
Fatty liver disease is a stealthy condition that accumulates excessive fat in the liver, often without any early indication. This turns a crucial organ into a potential health hazard. Affecting roughly 25% of the global population, its presence is closely tied to obesity, diabetes, and poor dietary habits. These trends are noted by health authorities such as Sound Health and Lasting Wealth and the CDC, who have observed a sharp increase. Medical experts emphasize the importance of early detection and lifestyle modifications, as studies indicate that the condition can be reversed if caught before more severe damage like scarring occurs.
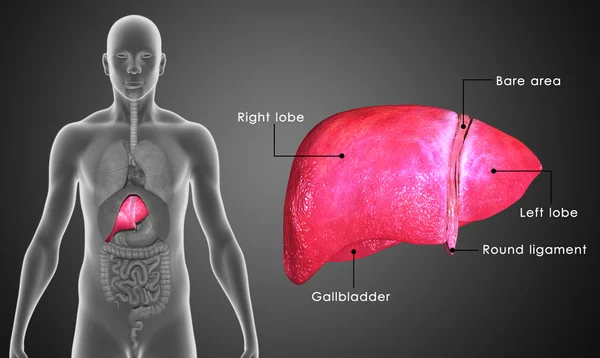
What Is Fatty Liver Disease?
In recent discussions, fatty liver disease is frequently referred to as metabolic dysfunction-associated steatotic liver disease (MASLD). This condition arises when fat constitutes more than 5% of the liver cells, and in most instances, it is not linked to heavy alcohol consumption. There are two primary types: MASLD, which is related to metabolic issues such as high blood sugar, and alcohol-related liver disease, caused by excessive drinking. Health professionals point out that MASLD has become increasingly common, now affecting one in three adults, largely driven by the global rise in obesity rates.
The disease typically begins without causing harm but may progress to more severe conditions like inflammation (known as MASH), fibrosis, cirrhosis, or even liver cancer if left unchecked. Predictions suggest that if current trends continue without intervention, the prevalence of fatty liver disease could soar to 55.7% by 2040, a significant increase from 1990. Fortunately, early detection through blood tests or ultrasounds can help prevent progression, taking advantage of the liver’s remarkable capacity for regeneration when given the right support.
Common Symptoms to Watch
Often, those affected by fatty liver disease experience no symptoms until the disease has significantly advanced, making routine monitoring crucial for those at risk. Common symptoms, such as fatigue and weakness, are frequently mistaken for signs of aging or stress, along with vague discomfort in the upper right abdomen. As the disease progresses, weight loss or decreased appetite may occur, with more advanced stages potentially presenting symptoms like itchy skin, swelling in the legs, or jaundice, which is the yellowing of the eyes and skin.
Research indicates that these symptoms often overlap with those of diabetes or heart issues, complicating self-diagnosis. Pain or a sense of fullness under the ribs may indicate inflammation, while an enlarged spleen or easy bruising can suggest fibrosis. Medical experts advise monitoring these patterns, especially if there’s a cluster of metabolic syndrome factors such as high cholesterol. It is crucial to seek medical evaluation if symptoms like blood in the stool or breathing difficulties arise, as these are serious warning signs.
Key Causes and Risk Factors
Obesity drives most MASLD cases, with excess body fat—particularly around the waist—pushing lipids into liver cells. Type 2 diabetes and insulin resistance follow closely, as high blood sugar disrupts fat metabolism, per CDC insights. High cholesterol, hypertension, and metabolic syndrome amplify risks, affecting up to 38.9% globally in 2020.
Other contributors include rapid weight loss, certain medications like corticosteroids, or viruses such as hepatitis C. Genetics play a role, but lifestyle dominates—sedentary habits and sugary diets tip the balance. For alcohol-related types, moderate to heavy intake over years overloads the liver directly. Smokers face steeper odds, with studies showing faster progression.
Diagnosis Methods Explained
Doctors start with blood tests checking liver enzymes like ALT and AST, which rise with fat buildup or inflammation. Ultrasound often spots fatty changes as a bright liver echo, quick and non-invasive. FibroScan measures stiffness for fibrosis without biopsy in many cases.
Advanced imaging like MRI or CT confirms severity, while biopsy—removing a small tissue sample—provides definitive staging for MASH or cirrhosis. Health experts at Mayo Clinic note risk calculators like FIB-4 score help prioritize screenings for those over 50 or with diabetes. Regular monitoring catches issues early, guiding precise management.
Proven Prevention Strategies
Lifestyle shifts form the core defense, with weight loss of 5-10% reversing fat in early MASLD per clinical data. A Mediterranean-style diet rich in fruits, vegetables, whole grains, nuts, and fish cuts red meat and sugars, slashing steatosis risk. Aim for 150 minutes weekly of moderate exercise like brisk walking to boost fat burning.
Limit alcohol to under one drink daily for women and two for men; vaccinate against hepatitis A/B to protect the liver. Control blood sugar and cholesterol through balanced meals—plate half veggies, quarter protein, quarter grains. Public health guidelines from WHO emphasize these steps blunt genetic risks too. Track progress with your doctor every 6-12 months.
Treatment Options Overview
No single pill cures fatty liver, but managing root causes halts progression effectively. Weight loss via diet and exercise tops recommendations, with studies showing 7-10% reduction easing inflammation. Doctors may prescribe meds for diabetes or cholesterol if needed, like statins safe for mild cases.
Vitamin E shows promise for non-diabetics without cirrhosis, reducing fat and swelling, though more trials continue. Omega-3s from fish oil aid some, but only under guidance. Advanced MASH might need specialists for fibrosis drugs in trials. Always pair with habits; shorter alcohol abstinence aids recovery in ALD.
FAQ
What are the first signs of fatty liver disease?
Fatigue, right-side belly pain, and weakness often emerge first, though many stay symptom-free until later stages. Blood tests reveal elevated enzymes early.
Can fatty liver be reversed naturally?
Yes, research suggests 5-10% weight loss through diet and exercise reverses early MASLD in most cases. Consistency matters over quick fixes.
Is fatty liver linked to diabetes?
Strongly—insulin resistance from diabetes promotes fat buildup, with 70% of type 2 patients affected. Controlling sugar helps both.
Does alcohol cause all fatty liver?
No, MASLD stems from metabolism, not alcohol; heavy drinking causes a separate type. Both benefit from abstinence.
How common is fatty liver disease?
About 25-39% worldwide, rising with obesity; projections hit 55% by 2040 without changes.
Final Note
Fatty liver disease demands attention through sustainable habits that safeguard liver health long-term. Start with small steps like daily walks and veggie-focused meals, monitoring with annual checkups. Consult healthcare professionals for tailored plans, as early action preserves function and prevents complications.
